More than 96 percent of hospitals in the US use an EHR system. The Electronic Health Record system is a core component in a hospital's IT ecosystem , where patients book appointments, receptionists manage schedules, and physicians access patient charts. In addition to all that, EHR systems can compile prescriptions and send them to pharmacies, receive lab results, prepare insurance claims, and so on.
When EHRs were first introduced in the 70s, they were a godsend. But today, people on the forefront of the industry are struggling to use the technology. Why is that? And how can we make EHRs more convenient and effective?
HHS - the US Department of Health and Human Services - can help by reducing the regulatory burden related to EHR.
Standard development organizations like Health Level 7 can introduce simple practices for adopting standardized content and data exchange specifications.
CMS - the Centers for Medicare & Medicaid Services - can work towards increasing interoperability and secure data exchange.
Health IT developers like EHR vendors and other industry experts can implement decisions of regulatory bodies and align them with hospital staff.
Of course, vendors and developers are the parties that can reduce the EHR burden from within. We will explore how they can address each of the EHR challenges today, specifically by tackling three issues: improving the clinical documentation process, usability, and public health reporting.
Another type of documentation - documentation for medication approval - is exchanged between healthcare providers, so they need to be compliant with industry-recognized standards.
Clinicians not only have to fill this documentation, but also comply with different sets of guidelines, and that cuts into their patient and personal time. Here’s how EHRs can help with that.
So, as recently as in 2020, CMS introduced new policies for E/M documentation. Now, patient history and physical exams are not required elements of patient visit docs, and outpatient visits have a much simpler procedure - a patient can fill in the form directly. New policies also clarified the use of patient history information - now it doesn’t need to be recorded all over again and should simply be reviewed and updated if needed.
To experience the benefits of these and many other revisions, you need to actually adopt them within the EHR. This process includes:
Standards like HL7 Fast Healthcare Interoperability Resources (FHIR) describe the unified workflow for a dozen different use cases. Their templates can be implemented by RESTful APIs connecting external Clinical Decision Support services and their clients (EHRs themselves).
Another program promoting interoperability includes the CMS’ Center for Program Integrity that has templates you can implement in your EHR to help with Medicare data collection.
CMS also has a pilot program for secure Medicare data exchange called the Electronic Medical Documentation Interoperability Initiative. The program is consistent with HL7 and HIPAA standards and basically helps organizations and IT vendors implement technical specifications better and faster.
ONC’s SAFER Guides have checklists for different EHR functions, describing how they should be organized and where you should look for the correct data format. For example, one of their recommendations is to run the dose range check before dispensing medication orders, which should reduce the risk of overdose.
Set up automatic processing of PDMP requests - a patient’s demographic information is automatically passed from EHR to PDMP.
Establish formatted reports for PDMP data - PDMP data is always displayed in a formatted, user-friendly, and unified manner.
Set up automatic PDMP data storing - medication history is automatically recorded in a patient’s log.
The main challenge for implementing PDMP sharing in the EHR workflow today is a regulatory one. Medication history is, of course, extremely sensitive information and should be protected. So, EHRs and hospitals themselves must ensure that the information they obtain and store is well protected - meaning, they must be subject to HIPAA.
ePrescribing is often available out of the box along with EHR systems, but there are mandates in place in different states to require DEA-certified CPOE by January 2021.
If they’re acquiring the first EHR system or switching to a different vendor, they should approach implementation effectively and consider staff burnout from the beginning. This includes:
When EHRs were first introduced in the 70s, they were a godsend. But today, people on the forefront of the industry are struggling to use the technology. Why is that? And how can we make EHRs more convenient and effective?
The EHR burden
Most difficulties EHR users (physicians, nurses) have are regulatory and administrative. Frontline healthcare staff have to comply with an ever-growing list of requirements, unfortunately, leading to their inability to provide the best patient care that can compromise the whole healthcare system. The Office of the National Coordinator for Health Information Technology (ONC) that leads the adoption of health technology in the US, highlights these EHR challenges.- Capturing clinical documentation increases the burden of day-to-day operations.
- EHRs have poor usability due to lack of coordination with actual clinical workflow.
- Accessing and extracting data for EHR performance reporting is problematic; requirements are often misaligned with federal programs.
- There is a lack of interoperability and automation with drug monitoring programs.
HHS - the US Department of Health and Human Services - can help by reducing the regulatory burden related to EHR.
Standard development organizations like Health Level 7 can introduce simple practices for adopting standardized content and data exchange specifications.
CMS - the Centers for Medicare & Medicaid Services - can work towards increasing interoperability and secure data exchange.
Health IT developers like EHR vendors and other industry experts can implement decisions of regulatory bodies and align them with hospital staff.
Of course, vendors and developers are the parties that can reduce the EHR burden from within. We will explore how they can address each of the EHR challenges today, specifically by tackling three issues: improving the clinical documentation process, usability, and public health reporting.
1. Implement seamless documentation flow
A clinic processes a ton of documentation. Most of it records information about the patient and the provided care (known as evaluation and management (E/M) documentation), which is important not only to monitor the patient’s health, but also to ensure accurate payment for services and insurance coverage.Another type of documentation - documentation for medication approval - is exchanged between healthcare providers, so they need to be compliant with industry-recognized standards.
Clinicians not only have to fill this documentation, but also comply with different sets of guidelines, and that cuts into their patient and personal time. Here’s how EHRs can help with that.
1.1. Adopt the latest policies for E/M documentation
Today, most EHR providers make detailed document templates so that all the information needed for audit is recorded. But this means that healthcare workers are required to record all this information, even when it’s not affecting care right now. And the volume of data these detailed forms create is so big that finding relevant information is difficult.So, as recently as in 2020, CMS introduced new policies for E/M documentation. Now, patient history and physical exams are not required elements of patient visit docs, and outpatient visits have a much simpler procedure - a patient can fill in the form directly. New policies also clarified the use of patient history information - now it doesn’t need to be recorded all over again and should simply be reviewed and updated if needed.
To experience the benefits of these and many other revisions, you need to actually adopt them within the EHR. This process includes:
- Making patient history information available from other systems using secure APIs
- Updating EHR design to support data verification instead of recording
- Creating new electronic workflows for a patient’s portal
1.2. Introduce interoperability standards
While health IT solutions streamline the administrative processes, they also create a large discrepancy, each one developing different interfaces that clinicians need to learn and get used to. So, we need to make different systems work together seamlessly and also help end users operate them with ease. Here are some options.Standards like HL7 Fast Healthcare Interoperability Resources (FHIR) describe the unified workflow for a dozen different use cases. Their templates can be implemented by RESTful APIs connecting external Clinical Decision Support services and their clients (EHRs themselves).
Another program promoting interoperability includes the CMS’ Center for Program Integrity that has templates you can implement in your EHR to help with Medicare data collection.
CMS also has a pilot program for secure Medicare data exchange called the Electronic Medical Documentation Interoperability Initiative. The program is consistent with HL7 and HIPAA standards and basically helps organizations and IT vendors implement technical specifications better and faster.
2. Introduce consistent and industry-specific UX
Implementing an enterprise system of EHR’s scale is an extremely complex task, mostly because people developing it are not the end users. And actual end users are rarely engaged. Developers have to better understand routines of healthcare providers and create an environment that supports existing workflow, instead of creating an additional one.2.1. Align EHR and clinical workflows
Unfortunately, EHRs are not always designed to support the existing workflow in the clinic. The Electronic Health Record Association developed a framework called Design Patterns for Patient Safety, where they explain best practices for EHR design in four areas:- Medications - how medication information is displayed, where to source content, and even what spacing to use
- Alert fatigue - designing smarter system alerts so they won't be ignored
- Laboratory results - recommendations for results presentation, grouping, and consistency
- Numeric display - setting a standard for recording numeric data
- Text display and layout - learning to effectively use the limited space to make information clear at first glance
- Consulting with end users when making decisions about displayed elements, alerts, the level of personalization, and so on
- Studying clinicians’ routines and work patterns and conducting interviews with them
- Optimizing third-party applications that clinicians already use
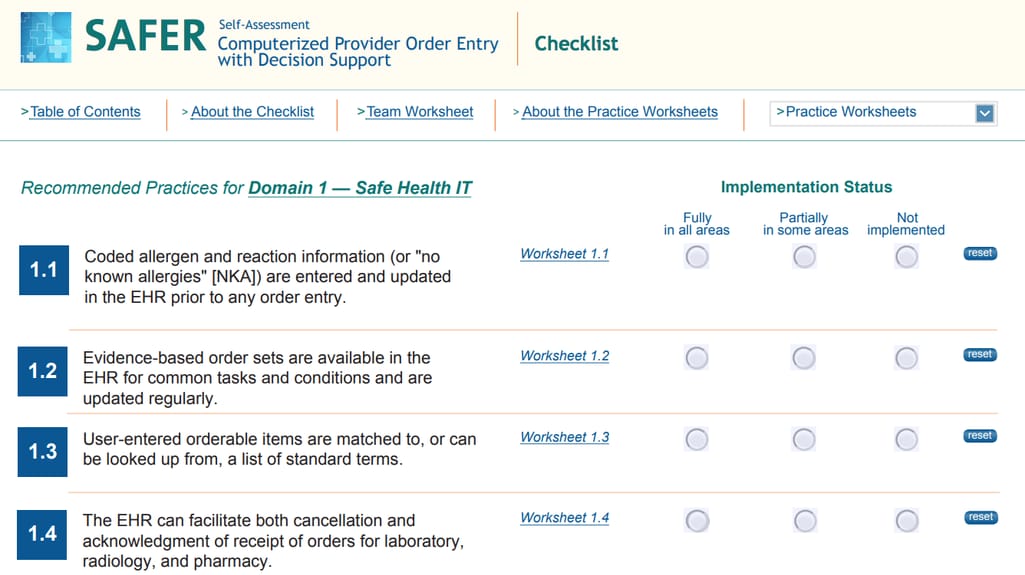
2.2. Standardize content across the whole system
Disparate content is a big problem in any system that consistently gets information from different sources. In EHRs, it means that a medication may have a different name in an order form and in a prescribing form. How to avoid confusion? First, by applying standards that help optimize how information is displayed.ONC’s SAFER Guides have checklists for different EHR functions, describing how they should be organized and where you should look for the correct data format. For example, one of their recommendations is to run the dose range check before dispensing medication orders, which should reduce the risk of overdose.
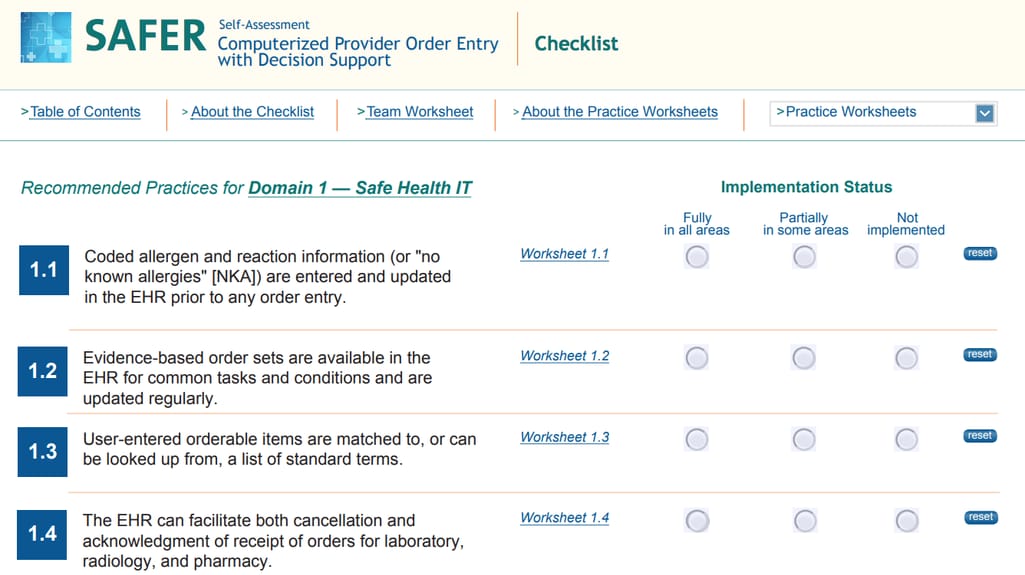
An excerpt of SAFER checklist for order entry Source: SAFER CPOE guide
SAFER explains that to do that, you need access to a dosing database like Databank or DailyMed, have info about a patient’s age and condition, and also dose limits for appropriate age, weight, etc. Developers can make data sources available and display them conveniently to reduce the time or number of clicks needed for a doctor to access this information.3. Integrate with PDMP and EPCS for better public health reporting
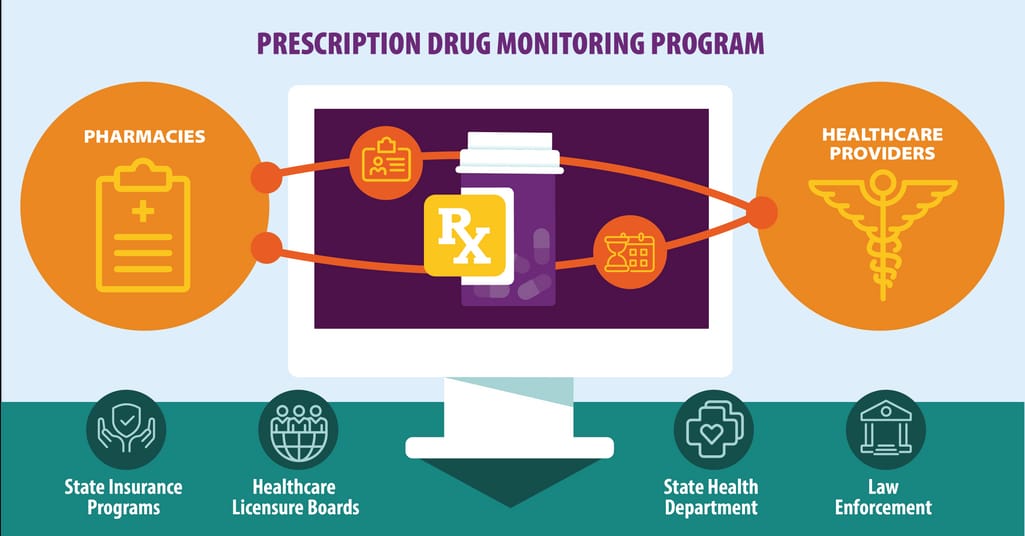
EHRs are one of the main sources of public health data. Statistics about births, deaths, and its causes, reports about laboratory results, and more recently - the number of cases of COVID-19 are all especially important data for public health agencies. Today, not all hospitals can effectively collect and share that knowledge: Some are not compliant with data privacy rules by HIPAA while others lack seamless integration with external systems. Here are some focal points EHR developers should consider.3.1. Integrate with PDMPs
Prescription Drug Monitoring Programs (PDMPs) control drug prescriptions making sure that patients are not misusing or overdosing from them. In short, clinicians can look up a patient's medication history and identify high-risk cases. During the current opioid epidemic, adopting PDMPs among healthcare providers is one of the main tasks of HHS. How to make this integration fast and effective?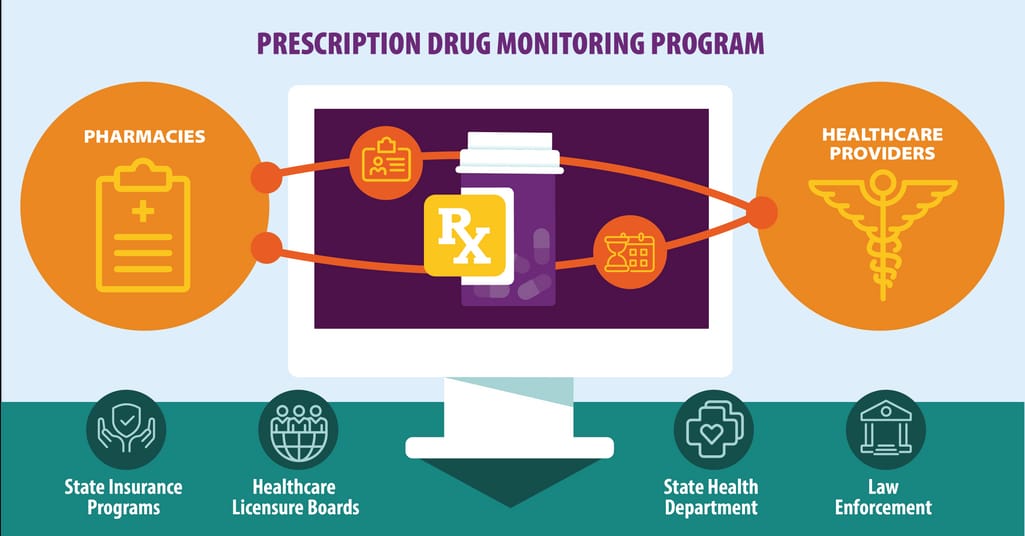
How drug monitoring works
Source: CDC
Set up automatic PDMP data access - an EHR should be able to access medication history automatically when a doctor writes a prescription or a patient is being admitted to the ER.Set up automatic processing of PDMP requests - a patient’s demographic information is automatically passed from EHR to PDMP.
Establish formatted reports for PDMP data - PDMP data is always displayed in a formatted, user-friendly, and unified manner.
Set up automatic PDMP data storing - medication history is automatically recorded in a patient’s log.
The main challenge for implementing PDMP sharing in the EHR workflow today is a regulatory one. Medication history is, of course, extremely sensitive information and should be protected. So, EHRs and hospitals themselves must ensure that the information they obtain and store is well protected - meaning, they must be subject to HIPAA.
3.2. Get total HIPAA compliance
There’s a difference between a HIPAA-compliant EHR and total compliance of a healthcare organization. Most popular EHR vendors are HIPAA-compliant - they should be to ensure the interoperability. But what does it mean for a hospital to be compliant with HIPAA?- Everyone involved with HIPAA compliance responsibilities should have clear roles and authorization levels
- Access to systems where sensitive data is stored should be protected with passwords
- Patient information should be encrypted
- Computer terminals should be physically guarded
- Each change in the system should be tracked and logged
3.3. Integrate with CPOE
Electronic prescribing of controlled substances (also called ePrescribing) is another technology helpful in fighting the opioid epidemic. But EPCS-compliant software also streamlines communication between prescribers and pharmacies. It's called computerized provider or physician order entry or CPOE. Not only is it faster to send electronic forms, helping pharmacies process the request right away, it also makes sure that the patient receives the dose as soon as possible and never misses it.ePrescribing is often available out of the box along with EHR systems, but there are mandates in place in different states to require DEA-certified CPOE by January 2021.
Shaping a new electronic environment
The big reason that many physicians feel the burden of using EHRs is because they were introduced to the system after it had already been implemented in the clinic. Today, the main technical task for healthcare providers is to learn by mistakes.If they’re acquiring the first EHR system or switching to a different vendor, they should approach implementation effectively and consider staff burnout from the beginning. This includes:
- Understanding the goal for implementation and establishing success metrics
- Creating workflow together with end users
- See what interoperability standards are getting traction in their state and work on adopting them
- Audit the clinic and conduct interviews with the staff
- Evaluate the standards lacking in day-to-day operations
- Try rolling into pilot programs by HHS and ONC to facilitate the use of new technology

Maryna is a passionate writer with a talent for simplifying complex topics for readers of all backgrounds. With 7 years of experience writing about travel technology, she is well-versed in the field. Outside of her professional writing, she enjoys reading, video games, and fashion.
Want to write an article for our blog? Read our requirements and guidelines to become a contributor.

