In the world of regulatory compliance, nothing happens fast. Back in 2016, the 21st Century Cures Act required that by January 1, 2020 all states implement an Electronic Visit Verification solution for personal care services. Forty-nine states plus Guam and the District of Columbia applied for the deadline extension, moving it out another year.
It’s been over two years since the initial date and some states still haven’t finished implementing EVV. Although Home Health Care Services (HHCS) have some time before their deadline in 2023, history tells us that most providers come in late.
Adopting new practices and technologies is never easy. Take a look at interoperability -- another healthcare industry concern with slow implementation speed. EVV raises a lot of questions and issues. Let’s discuss them and help you create a plan for smooth EVV adoption.
What is EVV? All you need to know
Electronic Visit Verification (EVV) is technology that allows for tracking caregiver visits. Created in response to massive volumes of healthcare fraud in home care services, the EVV program requires all Medicaid-funded home care agencies to implement a solution for verifying that a patient received the care that they needed. Specifically, this includes recording such information as:
- type of service performed,
- person receiving the service,
- date of the service,
- location of the service delivery,
- person providing the service,
- time the service begins and ends.
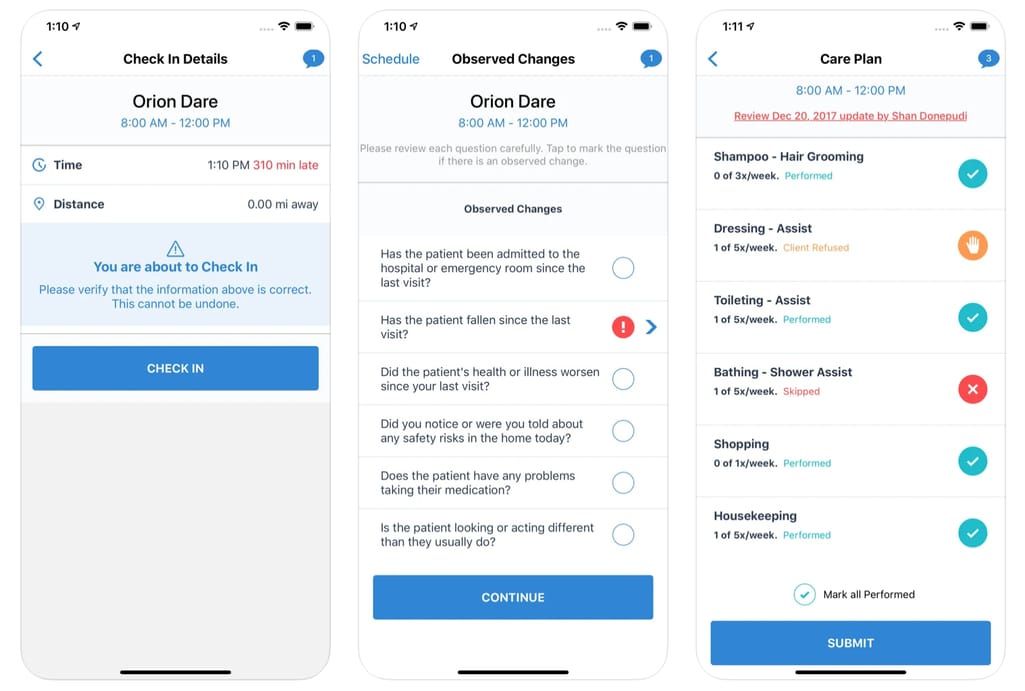
EVV mobile app functionality Source: CareBridge
While many agencies already use legacy systems for EVV tasks or rely on their EHRs to electronically document visits, they won’t be automatically compliant with the mandate. We will talk more about requirements for compliance.
Who is affected by EVV? As CMS puts it, “All services requiring an in-home visit that are included in claims under the home health category or personal care services category on the CMS-64 form are subject to the EVV requirement.” So, as long as your personal care or home health services are reimbursed by Medicaid or Medicare, your agency is subject to EVV requirements. If you want more details, visit your state’s Medicaid website to see the full list of Medicaid programs requiring the use of EVV.
Who isn’t affected by EVV? According to CMS, “Personal care services that are provided to inpatients or residents of a hospital, nursing facility, intermediate care facility for individuals with intellectual disabilities, or an institution for mental diseases, and personal care services that do not require an in-home visit, are not subject to the EVV requirement.” EVV also doesn’t apply when the provider and patient live together.
When is the compliance deadline? Personal care services were required to have an EVV system implemented by January 1, 2020. The states that failed to comply by this time and don’t have unavoidable delays are subject to incremental funds reductions of up to 1 percent a year. Home health care services must be implemented before January 1, 2023 with the same penalties. For more compliance information, make sure to read this FAQ document.
What’s in it for agencies? While you don’t have a choice to comply with EVV, this doesn’t mean that the new system brings only negative disruption. Some benefits to home health agencies include:
- faster medical billing and payments due to eliminated paperwork and reduced errors,
- better scheduling and communication thanks to a comprehensive tool,
- reduced fraud and help with audits with always available data.
Now, with all the bases covered, let’s talk about what EVV solution agencies will need to adopt. The federal mandate provided the states with ability to make two important choices themselves:
- the EVV implementation model deciding which party (the state or the agency) will have to choose/build an EVV system and pay for it,
- the EVV data collection model that determines how a caretaker will be submitting data.
EVV vendor models
There are five models for implementing an EVV system. The difference lies in how strongly the state wishes to be involved in vendor selection and system management.
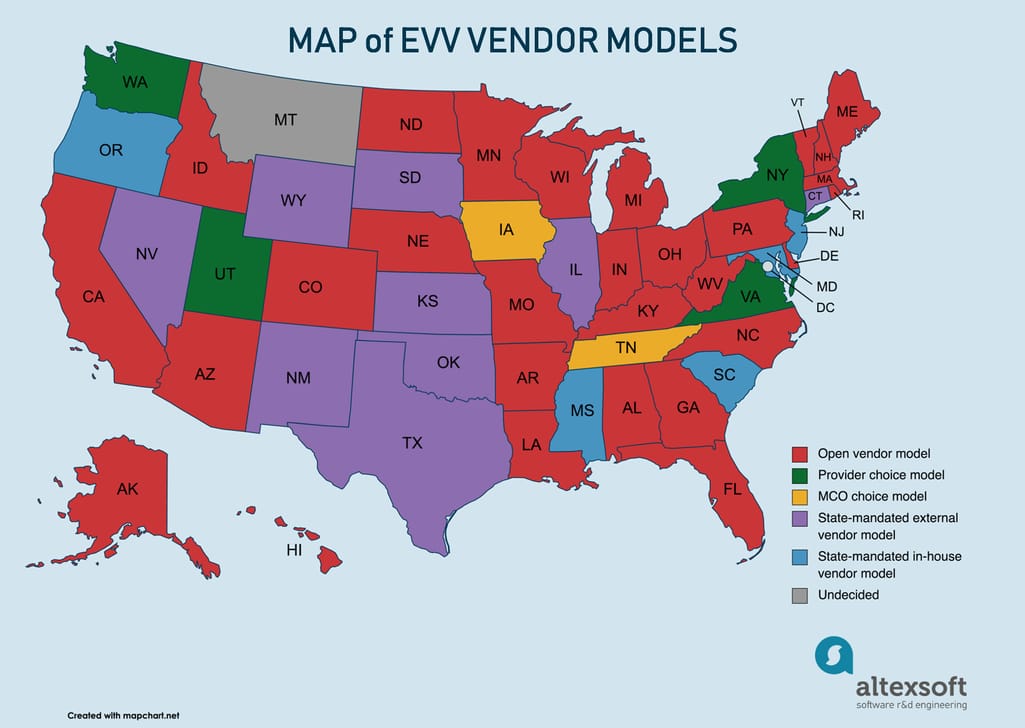 Overview of states and their EVV vendor models
Overview of states and their EVV vendor models
Open vendor. Under the most flexible model, agencies can either use an EVV vendor selected by the state, which will be free of charge, or they can work with a different vendor at their own expense, as long as their EVV solution passes certification criteria. This is friendliest choice both for agencies that didn’t have an EVV system before and those who already have one set up independently or within their EHRs. Under this model, states will also require an aggregator system that will be able to integrate all EVV data and will set requirements and standards for vendors to be able to connect with an aggregator.
States that selected the Open vendor model (and have chosen vendors): Alabama (HHAeXchange), Alaska (Therap), Arizona (Sandata), Arkansas (AuthentiCare), California (TBA), Colorado (Sandata), Delaware (TBD), Florida (Tellus), Georgia (Tellus), Hawaii (Sandata), Idaho (Sandata), Indiana (Sandata), Kentucky (Tellus), Louisiana (SRI), Maine (Sandata), Massachusetts (Optum), Michigan (state-run system), Minnesota (HHAeXchange), Missouri (Sandata), Nebraska (Tellus), New Hampshire (TBD), North Carolina (Sandata), North Dakota (Therap), Ohio (Sandata), Pennsylvania (Sandata), Rhode Island (Sandata), Vermont (Sandata), West Virginia (HHAeXchange), Wisconsin (Sandata).
Provider choice. In contrast with the Open vendor model, here, providers must select a vendor or build an EVV system themselves. The state will set data collection requirements and standards and can provide a list of approved vendors for easier choice. To offset the expenses on purchasing or building EVV technology, states are allowed to incorporate these costs into the reimbursement rate calculation.
States that selected the Provider choice model: New York, Utah, Virginia, Washington.
MCO choice. This model is similar to the previous one, but managed care organizations (MCOs) select the vendor and pay for it instead of providers. If the state has multiple MCOs, providers might be required to learn to use several EVV systems, but they’re allowed to require administrative support.
States that selected the MCO choice model: Iowa, Tennessee.
State-mandated external vendor model. While the previous three models were “open,” meaning that they were giving some freedom of choice to organizations, the last two models are “closed,” ensuring better oversight over EVV compliance. According to the external vendor model, a state picks one EVV vendor and requires all MCOs, providers, and individuals to use it. While this model puts all financial burden on the state, it eliminates problems with data standardization and access. The state must also provide training to all affected parties.
States that selected the external vendor model (and have chosen vendors): Connecticut (Sandata), Illinois (Sandata), Kansas (AuthentiCare), Nevada (AuthentiCare), New Mexico (AuthentiCare), Oklahoma (AuthentiCare), South Dakota (Therap), Texas (can choose Vesta or AuthentiCare), Wyoming (CareBridge).
State-mandated in-house vendor model. This most burdensome option for states requires them to do complete development and management of an EVV system. While it might be the most expensive option, it makes sense for states that already have solid EVV solutions in place. Other benefits include the full control of data access and training.
States that selected the in-house vendor model: Maryland, Mississippi, New Jersey, Oregon, South Carolina.
At the time of writing this article, Montana remained the only state that hasn’t decided on the model yet, promising to select a vendor in late 2021.
As you might have noticed, the lion's share of states is operating on the Open vendor model. While it provides a lot of flexibility, it also burdens providers with finding the right vendor. Later in the article, we’ll outline a few steps and answer some concerns to make this process less painful.
Ways to collect EVV data
The CMS offers three methods of collecting EVV data for states to choose or they can use them all. Let’s talk about how they work and what states picked which.
Mobile or web app. An app, downloaded to the caregiver’s personal or corporate phone/tablet, captures the service period and the worker’s location via GPS. Apps often feature extra functionality, such as scheduling, routing, and more.
States that approve the mobile method: Alabama, Arizona, Arkansas, Colorado, Connecticut, Delaware, Florida, Georgia, Hawaii, Illinois, Indiana, Louisiana, Maine, Massachusetts, Nevada, New Mexico, Ohio, Oklahoma, Oregon, Pennsylvania, South Dakota, Texas, Washington, Wisconsin.
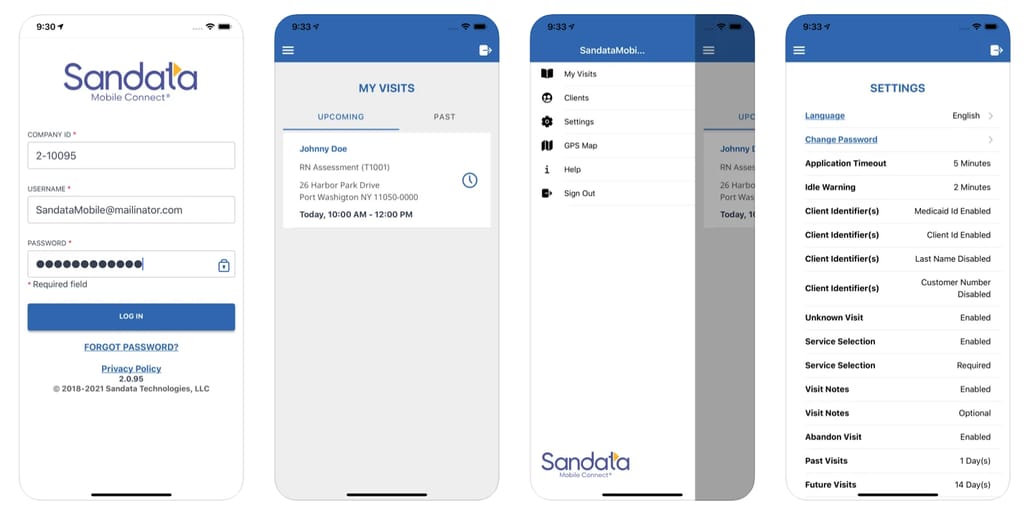
A mobile app of one of the most popular EVV vendors Source: Sandata
Telephony. Powered by interactive voice response (IVR) technology, the telephony method entails the caregiver using the client’s telephone (usually a landline) to call the 1-800 number, hear the automatic message listing the authorized services, select the ones they will be performing, and then call once again to clock out. Although this might be the easiest option in terms of implementation, it may present a problem if the service isn’t available due to disasters or malfunctions. Besides, it’s more vulnerable to fraud.
States that approve telephony: Alabama, Arizona, Arkansas, California, Colorado, Connecticut, Delaware, Florida, Georgia, Hawaii, Illinois, Indiana, Kansas, Maine, Maryland, Mississippi, Nevada, New Mexico, Ohio, Oklahoma, Pennsylvania, South Dakota, Washington, Wisconsin.
Fixed visit verification device. The least popular option, it requires installing a small device at a patient’s home. The device shows a code, which is updated every minute. When a caregiver arrives, they write down the displayed codes, and do the same when leaving. As soon as the worker has access to the EVV system, they log both codes in.

Example of a fixed verification device Source: Therap
States that approve fixed devices: Illinois.
Some states haven’t yet announced their preferred methods, though you may take part in the voting and discussion process posted on their EVV pages. Namely, this includes: Alaska, Idaho, Iowa, Kentucky, Michigan, Minnesota, Missouri, Nebraska, New Hampshire, New Jersey, New York, North Carolina, North Dakota, Rhode Island, South Carolina, Tennessee, Utah, Vermont, Virginia, West Virginia, Wyoming. Either way, you can be safe assuming that your state approves telephony and most likely approves mobile apps.
By this point, you’ve probably found your state on the EVV map and know what’s expected from you as a personal care or home health care provider. Now, let’s finally talk about compliance.
How to prepare for EVV software implementation
Since paths for implementation vary and don’t always depend on your choice, we can give you only foundational tips, pointing you in the direction where you need to research further. These directions will be impacted by three things:
- your state’s EVV vendor model,
- data collection types your state allows,
- your implementation deadline, varied by state.
Choose your vendor
If your state uses the state-mandated vendor model or MCO choice model, you can skip to the next part, since you don’t have to choose a vendor. Agencies operating in other states have to answer a few questions first.
Should I use the state system or choose one independently?
Adopting the state EVV is a great decision for many factors: It’s free and already complies with technical requirements, plus most state systems are industry leaders with rich functionality. The only solid reason not to use the state EVV is if you already have a solution that satisfies you and your employees. In this case, talk to your vendor or technology partner about smooth integration with the state system and certification. Consider the costs and time it will take to meet the requirements.
Should I pick an existing system or build a custom one?
“Buy vs build” is a common business conundrum. Getting a system out of the box is cheaper and faster to implement but you will need to research all the available options. (Hint: Your state likely provides a list of recommended vendors). Building a custom one is expensive and time consuming but you don’t need to settle for features available on the market. Instead, you can dictate your own rules, as long as they’re compliant with the mandate. Since for home health care services the deadline comes in 2023, you still have time to approach custom development.
What vendor should I choose?
You probably have your own parameters of what makes an EVV system perfect for you. But three main factors to consider are:
- interoperability with the state’s system and the agency’s other systems like EHRs (support for EDI transactions and API connectivity),
- EVV compliance according to the state’s standards and regulations (use the list of recommended vendors),
- ease of use for caregivers and admins (our article on assessing EHR usability might be helpful).
How to build a custom EVV system?
Since this is a loaded question, we recommend starting by looking at the popular systems on the market and noting what they lack, so you can cover that need with a custom solution. Involve staff in a conversation about features and usability, and further in testing. Look for a technology partner with expertise in healthcare applications and discuss with them the possibilities.
Choose a data collection method
Most states currently allow using both mobile apps and IVR systems so it’s safe to assume that undecided states will follow. But fixed devices remain a viable option, too, for example, as the last resort in case of poor signal. Ultimately, the choice depends on your initial goal.
- If you’re aiming just to reach EVV compliance, you may use telephony and fixed device options. They're simple, cheaper to implement, and traditional, so employees can easily get used to them.
- If you’re aiming to increase productivity, provide extra functionality, increase security, and reduce fraud, go for mobile apps. We want to cover them in detail.
Implementing Mobile EVV is easy with a vendor that provides an EVV app. Building a new EVV solution from scratch or expanding the functionality of the existing system might be too ambitious for a non-tech company. Yet there are pros to choosing mobile EVV over other data collection types.
- Convenience and user experience. Employees can clock in with a few taps rather than going through the phone call while a patient is waiting or manually logging in the code after the visit.
- Extended features. An agency is not limited to the functionality, which can go beyond the mandate requirements: Notifications, shift requests, scheduling, and easy communication with workers are some popular features.
One important consideration is that you will need to set up a mobile device policy. There are two options to consider:
- Bring-your-own-device model. One option is to allow caregivers to download an app on their personal phones, which is a less expensive approach since the agency only needs to pay the worker for the used data. But this policy presents a whole new set of problems: You have limited control over data security and integrity. Besides, some caregivers might not use smartphones or their devices can be old and laggy. Here, a second option might be a better choice.
- Corporate device. With a device picked and maintained by your IT team, you can ensure good user experience for all employees and wipe data remotely if the device was stolen. Plus, if the device is used for just one function, it will preserve the battery life.
Provide EVV training
Groups that will be using EVV directly need appropriate training. This includes workers who provide personal and home care services, agencies, fiscal employer agents, and program payers. If your state is responsible for picking EVV, they will keep you posted on when and how you can attend seminars.
On the contrary, provider agencies that are choosing vendors don’t just need to be trained but also know how to train their employees. Here are the main points your training should cover.
Basic EVV requirements and regulations. Explain what the federal mandate requires and the state’s position. Tell about consequences (penalties and sanctions) that follow noncompliance.
Benefits of EVV. Explain how the program will be preventing fraud and abuse, talk about new technological possibilities that will increase productivity, streamline claim processing, and even improve fuel reimbursements.
EVV software and hardware. Talk in detail about the system you plan to be using and how workers are expected to interact with it. Explain your device policy. Show how to use different features, the fixed verification device, etc. Tell them where they can go with technical issues.
Patient and family member responsibilities. Discuss how workers should communicate the new system to the clients and how the process will change for them.
Privacy and security concerns. Clearly communicate if the employees are being tracked via GPS or not. Eliminate any confusion about the technology, when it will be enabled, and discuss how you can eliminate the discomfort workers have with it. This is a great segue to the next section, where we want to talk about issues that workers and caretakers have with EVV and how to approach them.
Accounting for EVV concerns
Now when it’s clear what’s expected from home care providers, you probably have some apprehension about the program. And you wouldn’t be the first. Researchers from the University of California San Francisco interviewed personal care service workers and patients from states that already piloted the program and recorded their experiences. We want to list these concerns to help you prepare for problems you might have with your implementation.
Reduced quality of services
Visit verification can become a barrier between caregivers and clients. Having to check in immediately at arrival, workers sometimes have to sacrifice the patients’ needs to stay compliant. For example, if a person needs to use the bathroom at the start of a worker’s shift, clients must wait for them to clock in.
This lack of fluidity can be unrealistic. Caregivers often must keep to a strict schedule, when in reality, the start and end of a shift might change slightly to accommodate both parties. This adds unnecessary stress and makes workers rush on certain tasks or even clients, when a worker has several people to attend to in a day.
How to address it. Create a smooth login experience that would allow caretakers perform visit verification in a few minutes. Allow for flexible verification so people don’t feel pressured.
Technical and organizational problems
Issues with data capture and logging into the system, errors in recorded time, device malfunctions, lack of Wi-Fi, and other technicalities all add up to stress both for employees and patients. If a system breaks and doesn’t record the time consistently, this may exceed the consumer’s approved hour amount, resulting in higher receipts.
How to address it. Prioritize tech support and ensure people can access it via different channels such as phone calls and online chats. Make sure that all issues are solved and caregivers have alternative solutions. Provide convenient and user-friendly error correction functionality, so people can fix them immediately.
Privacy concerns
EVV systems must comply with HIPAA privacy and security requirements, but some concerns remain. For example, GPS is not required, but some states prefer to use it. Caregivers are uncomfortable with the feeling that they’re being surveilled. Workers also don’t feel confident entering the clients’ personal info such as social security numbers for identification and patients are fearing identity theft.
How to address it. Many of the concerns about privacy arise from the lack of understanding. Try to answer all of your workers’ questions about the use of data, explain why it’s required, and that there’s no better alternative. Or try to find an alternative if the requirements allow for it since the program does provide a lot of flexibility in how you approach visit verification.
Since there have been instances of workers leaving after the EVV rollout, be on the lookout for any problems that arise and try to accommodate your employees when possible. Remember that caregivers’ and patients’ convenience is just as important as EVV requirements.

Maryna is a passionate writer with a talent for simplifying complex topics for readers of all backgrounds. With 7 years of experience writing about travel technology, she is well-versed in the field. Outside of her professional writing, she enjoys reading, video games, and fashion.
Want to write an article for our blog? Read our requirements and guidelines to become a contributor.

